|
Dear colleagues: It has always been my hope that this newsletter would be used as a forum for exchange of experiences and ideas related to neural therapy. This month I would like to devote the entire issue to an interesting report from a reader (who incidentally I met at the Heidelberg neural therapy conference last July). Letter: Since you asked from a prior email, I will give details on a case of PGAS (Persistent Genital Arousal Syndrome): She was a retired professor around late 60 years in age, and had suffered with PGAS since her 30's. Over decades, she had sought out many specialists in the United States and abroad and tried all manner of treatment, without success. She came to me out of curiosity in that she had not seen an osteopath before, and asked if I could help in any way. From her history, I was intrigued that her symptoms began after a C-section and she had several C-section scars, one on top of the other. Moreover, the C-section scars were vertical midline scars, not commonly seen today. I had recently returned from the Heidelberg course and suggested that we try neural therapy, to which she agreed heartily. I injected her midline C-section scar on that first visit with a 30 gauge needle using less than 2ml of 1% lidocaine. She called from home a couple of hours afterward exclaiming excitedly that this was the first relief from the PGAS that she had experienced in 30 years! She returned two weeks later for another set of injections, and two weeks after that for a third round of injections, each time obtaining partial relief, and she seemed quite happy with that. However, she cancelled her fourth appointment stating that something conflicted in her schedule, and we have not seen her since. During the second visit, I had spoken to her that I would write up her case and publish it if any lasting effect be achieved and she was very encouraging. She also stated that I should contribute this treatment to a PGAS support website. I would like to write something and share it, hoping that neural therapy may help others with PGAS. However, I know neither her outcome nor why she stopped treatment. Were there side effects? Did another medical issue arise? Did she realize that PGAS was better than the absence of it, etc.? So this case is in limbo as far as publishing anything. Nevertheless, from this one case, I suspect that neural therapy could help other sufferers of PGAS. Theodore Jordan DO
My comments: Fascinating case. I once had an 80 year old female patient who mentioned (incidentally) unwanted sexual feelings in her genitalia but knew nothing about the condition and did not consider looking for an interference field! And I know exactly what you are talking about with the patient's seeming lack of interest in follow-up. I see this quite often, and sometimes wonder what is going through their heads. I have numerous cases in my files of patients with promising responses to neural therapy with whom I lose contact. I collect these as possible case histories for the newsletter, but many never see the light of day. Now a few items about PGAD from the literature: PGAD (formerly called PSAS or Persistent Sexual Arousal Syndrome) as a clinical entity is quite new. It was first described by psychiatrists Leiblum and Nathan in 2001. Since then at least 28 papers have been published. The cause is still unknown, but associations have been found with withdrawal from SSRIs and SNRIs, restless legs, irritable bladder, anxiety, increased soy intake in diet, small fibre neuropathy and Tarlov cysts. Waldinger and Schweitzer suggested renaming the disorder: Restless Genital Syndrome because of its overlapping symptoms with restless legs syndrome. Most of these associations suggest dysfunction at higher levels of the central nervous system. Restless legs are known to be associated with dysfunction in the basal ganglia and substantia nigra. And certainly sexual arousal is a complex process involving temporal and frontal lobes, cingulate gyrus, insula, basal ganglia, amygdala, hippocampus and probably other areas. Nevertheless, interference fields are known to provoke many complex pathophysiologies, neurological and otherwise. And as Dr. Jordan has demonstrated, treating one small nervous system locus of irritation can have profound effects even on complex processes. The "take-home" is always consider interference fields no matter how unusual or rare the medical condition.
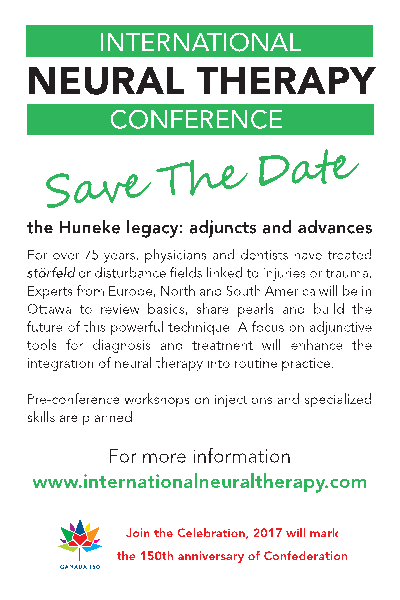
---------------------------------------------------------------------------------------------- We are now only four months from the first International Neural Therapy conference in North America. If you are considering attending, I would recommend that you register now and reserve your hotel room. Rooms will be in short supply this year as 2017 is Canada's 150th anniversary of Confederation and Ottawa will be busy.
--------------------------------------------------------------------------------------------- Third Heidelberg Neural Therapy Conference |
|
A free Spanish language neural therapy newsletter is available, published by D. David Vinjes of Barcelona, Spain at http://www.terapianeural.com/. Sign up at the site! Discussions are underway with regard to translating both English and Spanish literature. Feedback with regard to interest is invited from you, the readership of this newsletter. Your feedback is always welcome. |
| Contact Information
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~ email: drkidd@neuraltherapybook.comphone: 613-432-6596 web: http://www.neuraltherapybook.com ~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~ |